ORIGINAL ARTICLE | https://doi.org/10.5005/jp-journals-10067-0065 |
Psychosocial Interventions in Persons with Schizophrenia: A Protocol for Intervention Studies
1–3Department of Psychiatry, Government Medical College and Hospital, Chandigarh, India
Corresponding Author: Ashfaq A Dangroo, Department of Psychiatry, Government Medical College and Hospital, Chandigarh, India, Phone: +91 07006360294, e-mail: ashfaqad777@gmail.com
How to cite this article: Dangroo AA, Sahu KK, Arun P. Psychosocial Interventions in Persons with Schizophrenia: A Protocol for Intervention Studies. Ind J Priv Psychiatry 2020;14(2):75–79.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Background: Schizophrenia is a severe and chronic illness that is often the most difficult to manage, which has health and economic consequences for patients, families, and communities. Psychosocial interventions aim to change psychological, social, physiological, and functional outcomes by utilizing psychological or behavioral actions.
Methods: We hypothesize that psychosocial intervention offered to patients with schizophrenia to predict the outcomes of intervention. The research design of the study was a prospective intervention study in which intervention was given to patients at the outpatient department of the Department of Psychiatry, Government Medical College and Hospital, Chandigarh. Fifteen persons with schizophrenia (F20.0–20.9) as per the International Classification of Diseases-10 were consecutively included in this study. The intervention was done in eight sessions around 1 hour in each session on a weekly basis in 2 months.
Expected outcomes: This study is expected to predict the outcomes of the intervention and also helps the department to make interventions appropriate. These sessions along with pharmacological treatment improve the level of functioning and quality of life.
Significance: Psychosocial therapies that are added to antipsychotic medications that have been empirically validated target one or more deficit areas, such as positive and negative symptoms, cognitive impairments, and poor social functioning.
Trial registration: Clinical Trial Registry India CTRI/2021/01/030487. Registered on January 15, 2021.
Keywords: Psychosocial, Psychosocial interventions, Schizophrenia.
INTRODUCTION
Psychosocial interventions capitalize on psychological or social actions to produce a change in psychological, social, biological, and/or functional outcomes.1 Psychosocial intervention carries many approaches and methods, which bring a change in three areas that are symptoms, functioning, and well-being. The psychosocial interventions are provided in various settings that include outpatient clinics, primary care clinics, schools, client homes, hospitals and other facilities (including inpatient and partial hospital care), and community settings. Many interventions use a combination of office-based and naturalistic sites, and some are designed for specific environments.1
Some controversy has centered on the efficacy of formal psychosocial treatments for schizophrenic Indian patients and their families. In many underdeveloped countries, families have not received the benefits of evidence-based psychosocial intervention, and structured family interventions are costly and time-consuming, which makes them unsuitable for countries like India where there is the shortage of qualified staff and mental health facilities. The effect of structured intervention creates a progressive shift, and families learn to incorporate the knowledge and skills that they have been taught into their daily handling of the patient.2
Brief psychosocial interventions are intended to treat people with not only alcohol dependency but other serious psychiatric illnesses, which usually require greater expertise and more effective clinical care. Persons with schizophrenia respond well to comprehensive therapy and to the kinds of community-based support provided by institutions to help societies. But these same individuals often need to be persuaded that they have a problem and need to seek help.3 Chronic illnesses such as schizophrenia often affect the lives of patients and their caregivers. Existing research indicates that a positive psychosocial environment has a positive influence on the outcomes of schizophrenia. Family functioning plays a crucial role in the treatment of the person with schizophrenia.4
The psychosocial interventions can occur in any format, for example, in groups or individually, and these interventions help the mental health providers to prevent relapses and increase treatment adherence in schizophrenia. Patients with schizophrenia and their families should expect support and have a right to have complete knowledge about the illness of the patient. Brief psychosocial intervention modules are adopted by psychiatric or medical professionals for families of schizophrenic patients in terms of change in the burden of care and the quality of life. The focus is not just on clinic-based interventions (including modeling, role playing, and social reinforcement), but also the setting of homework activities like exercises and activity scheduling the feasibility of the treatment.5
Psychosocial interventions may also seek to influence emotional expressions, such as family hostility and criticism in the family, and play an active role in containing and managing symptoms. The relapse rate ofpatients who are on medications is still 30 to 50%.6 In order to achieve the objective of community rehabilitation, it is important to clearly document the coping styles of schizophrenic patient and their family. Effective rehabilitation will improve the patient and at the same time deliver a better outcome. Time constraints as well as pessimistic outlook of many professionals regarding the treatment for schizophrenia have made therapeutic cycle lacking.6
REVIEW OF LITERATURE
The developing countries are lacking the evidence-based structured psychosocial interventions. Patient and caregivers of schizophrenia taking treatment from Postgraduate Institute (PGI) were psychoeducated in the study; the most impressive differences in the reduction of severity of psychopathology and increased perception of support among caregivers were noted.2 Living with a person suffering from schizophrenia is often challenging. The sessions comprised rapport building, education about the disorder, concept of expressed emotions and their role in outcome, role of key relatives and family, information about drugs and their side effects, compliance issues, information on access to clinical resources, problem-solving techniques/skills, and coping and communication skills.4 The antipsychotic medicines along with psychosocial intervention were the main instruments to maintain patient and prevent relapse rate, and reports suggested that self-coping in schizophrenia patients can control and improve the quality of life.6
There is scattered small-scale evidence suggesting that various psychosocial interventions may be a feasible intervention option for people with mild intellectual disabilities and a range of mental health problems, including depression, anxiety, and anger.7 Longer interventions showed a statistically significant impact on depressive symptoms and dichotomous depression outcomes compared with shorter interventions. The duration of interventions is of importance since interventions lasting for 3 months exhibited more positive effects compared with shorter interventions.8 The psychotic symptoms, psychological distress, information about the condition, and money were the four most common areas in which patients had needs and required assistance, whereas the four most common areas of needs reported by caregivers were psychological distress, money, company, and intimate relationships. The majority of schizophrenia persons’ needs remain unsatisfied.9,10
RATIONALE OF THE STUDY
Schizophrenia and related disorders are commonly associated with impairment in socio-occupational functions. Empirically validated psychosocial interventions, added to antipsychotic medication, target one or more of deficit areas, including positive and negative symptoms, cognitive deficits, and poor social functioning. Various unmet psychosocial intervention needs of persons with schizophrenia attending the psychiatric outpatient clinic were reported. There is a lack of evidence of psychosocial intervention service in a comprehensive manner, which addresses those unmet needs so this study was an attempt to fill the gap.
AIM AND OBJECTIVE
To study the psychosocial needs and outcomes of intervention in persons with schizophrenia.
MATERIALS AND METHODS
The research was designed as a pre- and post-study without a control group. It was a prospective intervention study, and the sampling was done by a consecutive sampling method. The study was carried out at outpatient department (OPD) of the Department of Psychiatry, Government Medical College and Hospital, Chandigarh. The total sample size was 15 persons with schizophrenia (F20.0–20.9) as per the International Classification of Diseases (ICD)-10.11 The subject recruitment procedure consisted of consecutive patients who gave written consent to participate in the study, and those who fulfilled inclusion and exclusion criteria were included in the present study.
SELECTION CRITERIA
Eligible Population
All patients who are diagnosed with schizophrenia (only F20.0–20.9) as per ICD-10,11 should be clinically stable, and defined as the absence of exacerbation of illness requiring an increase in drug doses by 50% in past 3 months were eligible.12 The age-group of the population should be 18 to 55 years. Schizophrenia patients with an illness duration of more than 1 year and less than 5 years and those who gave written consent to participate in the study were included.
Exclusion Criteria for the Patients
Patients should not be unstable or have any major medical illness or substance dependence (except nicotine and caffeine). Those who are already receiving psychosocial intervention in the OPD were excluded. The patient was excluded if he developed worsening of clinical condition while receiving psychosocial intervention.
ASSESSMENTS/TOOLS TO BE USED
- Sociodemographic and Clinical Data Sheet
- Detail psychosocial assessment
- Psychosocial Intervention Needs Checklist13
- Global Assessment of Functioning (GAF)14,15
- WHO-QoL-BREF16
- Morisky Medication Adherence Scale (MMAS)17
- Social Occupational Functioning Scale (SOFS)18
- Patient Satisfaction Scale (PAT-SAT)19
- Sociodemographic and Clinical Data Sheet: It was a semi-structured pro forma, including registration number, name, age, sex, educational level, age of onset, duration of illness, duration of treatment, whether ongoing psychosocial treatment, symptoms, subtype, number of hospitalization, and side effects of the patients with severe mental illness. Similarly, caregivers’ name, age, sex, education level, marital status, occupation, family monthly income, family size and type, domicile, and religion were included in the pro forma.
- Psychosocial Intervention Needs Checklist: This was developed for the present study based on the World Health Organization’s20 framework and three research tools—the Camberwell Assessment of Need—Research (CAN-R) by Phelan and Slade,21 Supplementary Assessment of Need Scale (SNAS) by Neogi et al.,22 and Screening Tool for Assessment of Psychosocial Problems (STAPP) by Sahu et al23 —which assess the areas of psychosocial dysfunctions or problems that require psychosocial intervention.
- Global Assessment of Functioning:The GAF is a 100-point scale divided into intervals or sections, each with 10 points. The GAF is a global evaluation of how a patient is doing and is designed to be a universal rather than diagnostic-specific scoring system. It covers the range from well‐being to severe psychopathology. Anchor points (verbal instructions) explaining symptoms and functions that are significant for scoring are included in the 10-point intervals. The scale is provided with examples of what should be scored in each 10-point interval. The present GAF is found as Axis V of the Internationally accepted Diagnostic and Statistical Manual of Mental Disorders, fourth edition text revision.14,15
- World Health Organization Quality of Life-BREF Hindi Version: WHO-QoL-BREF is an abbreviated 26-item version of the WHO-QoL-100 scale and was developed using data from the field trial version of the WHO-QoL-100. It was created in a cross-cultural environment and was available in over twenty languages. This instrument places primary importance on the perception of the individual. It is one of the best-known instruments to measure the generic QoL. It is a self-administered scale that measures the following broad domains: physical health, psychological health, social relationships, and environment. The Hindi version was developed and validated and is widely used in various mental illnesses.16
- Patient Satisfaction Scale: The scale comprises 19 items subdivided into six domains—trust, communication, exploration of ideas, body language, active listening, and miscellaneous. It receives a rating on a 5-point Likert scale (strongly agree, agree, do not know, disagree, and strongly disagree).19 Even persons with only a few years of school find the PAT-SAT to be easily legible and understood. From the patient’s perspective, the scale assesses the complicated and multidimensional interaction between the therapist and the patient. The PAT-SAT scale can be utilized without prior practitioner training and with little patient instructions. It has been translated into Hindi and used in the Indian setting.24
- Morisky Medication Adherence Scale: The eight-item MMAS is a self-report scale that is commonly used. It has been validated for the use in depression and physical conditions, such as hypertension and asthma. The strength of this questionnaire is its informality. It puts the patient at ease by acknowledging that many people face the same issues, thereby normalizing the responses.17
- Social Occupational Functioning Scale: This is a scale to assess social functioning in persons with severe mental illness. Social functioning refers to activities of daily living (personal care, hygiene, and grooming), communication and interpersonal skills, and social, leisure, and work-related activities. This scale has 14 items with each item representing a different domain of social functioning. Each item has five anchor points describing the level of impairment in increasing order of severity. Please read the general rating scale and the item description carefully before rating each item.18
Intervention
- Monitoring compliance for intervention through MMAS17
- Psychoeducation—IPS guidelines by Sarkhel et al.25
- Activity scheduling and monitoring
- Intervention to address impaired socio-occupational functioning as per initial assessment and monitoring with SOFS by Saraswat et al.18
- Engagement in Vocation or Productive Work
- Referral, guidance, and monitoring
- Pretest: An initial assessment of three cases would be conducted to check the suitability of the tools to be used in the study. The sequence of the intervention may be changed on case-to-case bases keep in view of the needs of case. The sessions will be later on planned as per the needs of the patients.
Description of Intervention Package and Plan
- Monitoring Compliance for Intervention: It will be monitored whether persons with schizophrenia are complying with both pharmacological and non-pharmacological treatment as prescribed by the clinician.17
- Psychoeducation
Goals of the Psychoeducation
- To ensure basic knowledge and competence of patients and their relatives about the illness.
- To provide insight into the illness
- To promote relapse prevention
- Engaging in crisis management and suicide prevention if required through referral services.
Essential Elements
- Briefing the patients about their illness
- Problem-solving training
- Communication training
- Self-assertiveness training (IPS guidelines 2020)25
- Activity Scheduling: To help persons with schizophrenia in scheduling various activities into a day-to-day lifestyle and help them to identify a timetable of activities to manage their attention, develop feelings of competence, and develop social confidence. A written format of activity is scheduled and is monitored in each session to examine whether persons with schizophrenia are maintaining it.
- Intervention to Address Impaired SOF as Initial Assessment: After assessing the SOF scale, a complete picture was found on the lacking area of persons with schizophrenia’s social occupational and functional life. As per requirement, these issues should be addressed.11
- Engage in Vocation or Productive Work: If person with schizophrenia is functional, then vocational counseling is needed in order to involve him/her in some productive activity, and once the client is ready, then we proceed for it. After assessing whether there is any kind of vocational help needed, she/he can be helped to engage in it.11
- Referral, Guidance, and Monitoring: In the psychosocial need checklist, there would be some needs which can be fulfilled by other agencies. The patient was referred for those services.
PROCEDURE
After receiving ethical clearance on August 13, 2020, those patients who attended to psychiatry OPD, diagnosed with schizophrenia (F20.0–20.9) as per ICD-10 criteria, met the inclusion and exclusion criteria, and gave consent for the study were initially assessed consecutively.
Sociodemographic and clinical details were collected from the case record file and from the patient or caregivers. A detailed psychosocial assessment was done; Psychosocial Intervention Needs checklist was administered, and based on that, psychosocial intervention needs were identified; GAF for overall functioning and WHO-QoL-BREF for quality of life were administered; SOFS was administered to check the socio-occupational dysfunction of the patient and the impaired areas were addressed in the intervention; and MMAS was used to check the compliance of the patient. Subsequently, sessions were planned as per the intervention package (psychosocial intervention) and were proceeded along with the routine treatment from the OPD.
All interventions in the package were not applicable for all the patients, they were specifically made for each person with schizophrenia depending upon the score of SOFS. Then, during intervention sessions, their issues were addressed as per the needs. Soon after the intervention, post-assessment was done assessing again on GAF, WHO-QoL-BREF, SOFS, MMAS, and additionally on PAT-SAT. (Fig. 1)
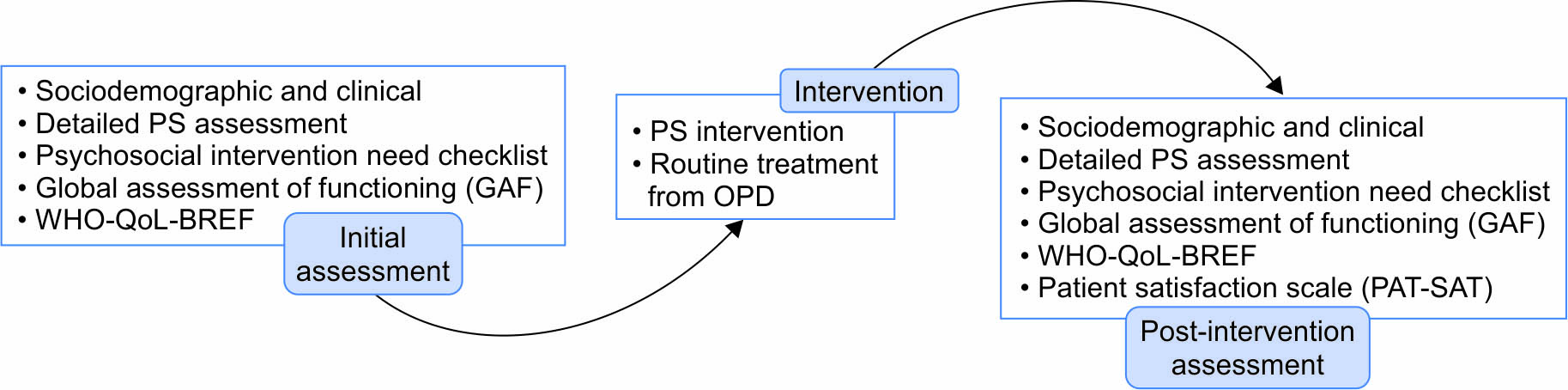
Fig. 1: Flow Chart of the Study
Primary Outcomes
There are two primary outcomes corresponding to the study hypothesis.
To improve the quality of life and socio-occupational functioning of the patients while addressing their needs during the intervention.
To check the compliance of the medication and treatment and improve their compliance medication as well as both phrenological and non-phrenological treatment.
Secondary Outcomes
This study is expected to reveal the outcomes of the intervention and also help in the department to make interventions appropriate. The stigma among the patients is reduced in intervention. The study showed the impaired areas of the patients, which were later on addressed in intervention. Patients enrolled in the study received vocational counseling and were engaged in appropriate referral services. The study also showed the importance of psychosocial treatments along with phraseological treatments and how psychosocial interventions play important role to the patients attending OPD clinics of hospitals in psychiatric settings.
Statistical Analysis
- Data collected were entered in the master chart and later analyzed using appropriate statistics with the help of Statistical Package for the Social Sciences (SPSS 16).
- Descriptive statistics—mean and percentage were used, and for association between variables, Pearson’s coefficient of correlation test was used, and comparative profile in pre- and post-intervention was done by using Wilcoxon signed-rank test.
DISCUSSION
The research protocol involves a psychosocial intervention plan for people working in the field of schizophrenia and enables to identify the needs of the patient on which the intervention plan is drafted. The key elements are, therefore, to access the patient’s psychosocial needs, manage patients in stable phase to improve their quality of life, and make adherent to medication. Interprofessional primary healthcare teams have aided in the creation and implementation of Canadian and American healthcare reform goals of enhancing access, quality of treatment, and availability of services to suit the demands of an increasingly complex patient population.26 Currently, no practice guidelines exist that can provide clarity to psychiatric social workers in the provision of mental healthcare within primary healthcare settings. It is, therefore, imperative to develop innovative strategies in psychosocial intervention treatments to increase access to a basic standard of guideline-informed mental healthcare.
Strengths and Limitations
The protocol strengths are that the intervention brings into line with recommendations from the manual working with people in schizophrenia and India’s National Mental Health Policy to develop innovative strategies that strengthen existing systems.27 It complements and builds on other research initiatives in India.28 It actively explores the challenges of implementing a complex intervention in “real world” settings, taking into consideration policy as well on the ground realities experienced by schizophrenia patients and community members. The evidence generated has potential to inform decision-making for system planners on a scalable solution to increasing access to high-quality interventions. The main study limitation is that although it was conducted in only psychiatric settings, the outcomes may only be generalizable to similar cultural contexts and settings.
DECLARATIONS
Ethics Approval and Consent to Participate
The purpose and the design of the study shall be explained to the patient and a close family member in the language they understand, viz. Hindi or English. The study was conducted with patients diagnosed with schizophrenia (only F20.0–20.9) as per ICD-10 attending the Psychiatry Outpatient Department of Government Medical College and Hospital, Chandigarh. A written and informed consent was taken from all. The patient and the consenting caregivers were informed that they could withdraw at any time from the study without giving reasons for the same. The confidentiality of the information obtained was maintained and revealed only to the faculties/editors of this study. The study is registered in ethical committee under registration GMCH/IEC/2020/327/98 on August 13, 2020.
Availability of Data and Materials
Any data required to support the protocol was made available by the Department of Psychiatry Government Medical College and Hospital, Chandigarh, and during the current study, patients already enrolled in the department for treatment were enrolled for the study.
ORCID
Ashfaq A Dangroo https://orcid.org/0000-0002-3192-2310
REFERENCES
1. England MJ, Butler AS, Gonzalez ML. Psychosocial interventions for mental and substance use disorders: a framework for establishing evidence-based standards. Washington (DC): National Academies Press (US); 2015.
2. Kulhara P, Chakrabarti S, Avasthi A, et al. Psychoeducational intervention for caregivers of Indian patients with schizophrenia: a randomised-controlled trial. Acta Psychiatr Scand 2009;119(6):472–483. DOI: 10.1111/j.1600-0447.2008.01304.x.
3. Babor TF, Higgins-Biddle JC. Brief intervention for hazardous and harmful drinking: a manual for use in primary care. World Health Organization, Document No. WHO/MSD/MSB/ 01.6b.2001.
4. Kumar R, Nischal A, Dalal PK, et al. Impact of brief psychosocial intervention on key relatives of patients with schizophrenia: a randomized controlled trial. Indian J Psychiatry 2020;62(2):137–144. DOI: 10.4103/psychiatry.IndianJPsychiatry_138_19.
5. Adams C, Wilson P, Bagnall AM. Psychosocial interventions for schizophrenia. Qual Health Care 2000;9(4):251–256. DOI: 10.1136/qhc.9.4.251.
6. Peter W, Lee H, Leih-mex F, et al. Coping strategies of schizophrenic patients and their relationship to outcome. Br J Psychiatry 1993;163:177–182. DOI: 10.1192/bjp.163.2.177.
7. Hatton C. Psychosocial interventions for adults with intellectual disabilities and mental health problems: a review. J Ment Health 2002;11(4):357–373. DOI: 10.1080/09638230020023732.
8. Forsman AK, Nordmyr J, Wahlbeck K. Psychosocial interventions for the promotion of mental health and the prevention of depression among older adults. Health Promot Int 2011;26 (Suppl. 1):i85–i107. DOI: 10.1093/heapro/dar074.
9. Kulhara P, Avasthi A, Grover S, et al. Needs of Indian schizophrenia patients: an exploratory study from India. Soc Psychiatry Psychiatr Epidemiol 2010;45(8):809–818. DOI: 10.1007/s00127-009-0126-1.
10. Grover S, Avasthi A, Shah S, et al. Indian Psychiatric Society multicentric study on assessment of health-care needs of patients with severe mental illnesses as perceived by their family caregivers and health-care providers. Indian J Psychiatry 2015;57(2):181–189. DOI: 10.4103/0019-5545.158185.
11. World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization; 1993.
12. Lobana A, Mattoo SK, Basu D, et al. Convergent validity of quality of life interview in an Indian setting: preliminary findings. Indian J Psychiatry 2002;44(2):118–124. PMID: 21206556; PMCID: PMC2954338
13. Singh J. Psychosocial intervention needs of persons with severe mental illness attending psychiatric out patient clinic [dissertation]. Chandigarh: Panjab University; 2019.
14. Endicott J, Spitzer RL, Fleiss JL, et al. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry 1976;33(6):766–771. DOI: 10.1001/archpsyc.1976.01770060086012.
15. Goldman HH, Skodol AE, Lave TR. Revisiting axis V for DSM-V: a review of measures of social functioning. Am J Psychiatry 1992;149(9):1148–1156. DOI: 10.1176/ajp.149.9.1148.
16. WHOQOL Group. Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med 1998;28(3):551–558. DOI: 10.1017/s0033291798006667.
17. Morisky DE, Ang A, Wood MK, et al. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens 2008;10(5):348–354. DOI: 10.1111/j.1751-7176.2008.07572.x.
18. Saraswat N, Rao K, Subbakrishna DK, et al. The Social Occupational Functioning Scale (SOFS): a brief measure of functional status in persons with schizophrenia. Schizophr Res 2006;81(2-3):301–309. DOI: 10.1016/j.schres.2005.09.008.
19. Hansen L, Vincent S, Harris S, et al. A patient satisfaction rating scale for psychiatric service users. Psychiatrist 2010;34(11):485–488. DOI: 10.1192/pb.bp.107.019067.
20. World Health Organization. Solving mental health problems. In: The World Health Report 2001: mental health: new understanding, new hope. World Health Organization; 2001. p. 59–64.
21. Phelan M, Slade M, Thornicroft G, et al. The Camberwell Assessment of Need: the validity and reliability of an instrument to assess the needs of people with severe mental illness. Br J Psychiatry 1995;167(5):589–595. DOI: 10.1192/bjp.167.5.589.
22. Neogi R, Chakrabarti S, Grover S. Health-care needs of remitted patients with bipolar disorder: a comparison with schizophrenia. World J Psychiatry 2016;6(4):431–441. DOI: 10.5498/wjp.v6.i4.431.
23. Sahu KK, Chavan BS, Bala C, et al. Reliability and validity of the screening tool for assessment of psychosocial problems. Open J Psychiatry Allied Sci 2019;10:163–168. DOI: 10.5958/2394-2061.2019.00039.9.
24. Das S, Gupta N, Debbarma A, et al. Profiling the initial 1st year cohort of patients utilizing a tertiary hospital-based geriatric mental health-care service using the “Service Evaluation Framework”. Indian J Soc Psychiatry 2018;34(1):37–47. DOI: 10.4103/ijsp.ijsp_117_17.
25. Sarkhel S, Singh OP, Arora M. Clinical practice guidelines for psychoeducation in psychiatric disorders general principles of psychoeducation. Indian J Psychiatry 2020;62(8):S319–S323. DOI: 10.4103/psychiatry.IndianJPsychiatry_780_19.
26. Ashcroft R, Kourgiantakis T, Brown JB. Social work’s scope of practice in the provision of primary mental health care: protocol for a scoping review. BMJ Open 2017;7(11):e019384. DOI: 10.1136/bmjopen-2017-019384.
27. Ministry of Health and Family Welfare, Government of India. New pathways new hope. National mental health policy of India. New Delhi: Ministry of Health and Family Welfare, Government of India; 2014. Available from: https://nhm.gov.in/images/pdf/National_Health_Mental_Policy.pdf [Accessed February 9, 2021].
28. Semrau M, Evans-Lacko S, Alem A, et al. Strengthening mental health systems in low-and middle-income countries: the emerald programme. BMC Med 2015;13:79. DOI: 10.1186/s12916-015-0309-4.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.